Among medicinal products an important placeoccupy antibiotics of the latest generation, active against many microbes. They are used to treat infectious pathologies, which significantly reduced the death rate of patients from today's commonplace pneumonia and pyelonephritis. Due to antibiotics, the flow is facilitated and recovery is accelerated with bronchitis, sinusitis, and also complicated surgical operations became possible. Even wound infections are successfully treated with antibiotics.
Antibiotics of a wide spectrum (ABSS)
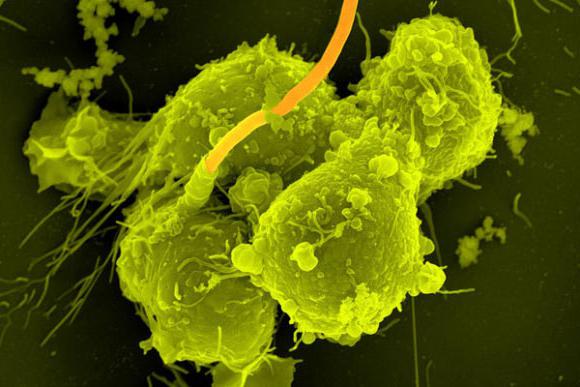
This category of antimicrobialsincludes substances active against gram-negative organisms and gram-positive organisms. The first are causative agents of intestinal diseases, inflammatory pathologies of the genitourinary and respiratory systems. Gram-positive organisms often cause wound infections and mediate the occurrence of postoperative complications in surgery.

List of ABSS of different release time
Some broad-spectrum antibioticsgenerations are also active against protozoal infections. An example are nitroimidazole derivatives - tinidazole, ornidazole and metronidazole. The most widely used metronidazole due to affordability. Its class analogue - tinidazole - is similar in the spectrum of antimicrobial activity, but it is not applied parenterally. In general, all groups of broad-spectrum antibiotics are presented as follows:
- natural penicillins;
- inhibitor-protected aminopenicillins;
- antisseinemic penicillins, including inhibitors;
- cephalosporins of the third generation, cephalosporins of the IV generation;
- group of aminoglycosides;
- antibiotics of tetracycline;
- macrolide antibiotics;
- antibiotics of a number of carbapenems;
- chloramphenicol;
- phosphomycin;
- rifampicin;
- Dioxydin;
- sulfonamides;
- quinolones, fluoroquinolones;
- group of nitrofurans;
- antibiotics of the nitroimidazole series.
This list does not list the group namesantibiotics of a narrow spectrum. They are specific for a small number of microbes and are effective against them. Narrow spectrum drugs can not be used for the treatment of superinfections and do not apply empirically. They are used as antibiotics of the first series with the established form of pathogen.

List of ABSS of recent generations
The above antimicrobial agentsrefer to a wide range of drugs. This is a complete list of groups of substances that have activity against gram-positive and gram-negative microbes. However, the list includes both the latest generation of antibiotics and the earlier members of the group. Among the above representatives of the latest generations are the following groups of drugs:
- beta-lactamase-resistant aminopenicillins (Sulbactam, Ampicillin, Clavulanate, Amoxicillin);
- cephalosporins of the III and IV generations ("Cefotaxime", "Cefoperazone", "Ceftazidime", "Ceftriaxone", "Cefpirim", "Cefepime");
- aminoglycoside antibiotics of the III generation (Amikacin, Netilmicin);
- 14- and 15-membered semi-synthetic macrolides (Roxithromycin, Clarithromycin, Azithromycin);
- 16-membered natural macrolide antibiotics ("Midecamycin");
- fluoroquinolones III and IV generations ("Levofloxacin", "Sparfloxacin", "Gatifloxacin", "Trovafloxacin", "Moxifloxacin");
- carbapenems ("Meropenem", "Imipinem-cilastatin", "Ertapenem");
- nitrofurans ("Nitrofurantoin", "Furazidin", "Ersefuril").

Antibiotics excluded from the list
These previously protected antisexpousicPenicillins have a wide spectrum of activity, however, they are used only against Pseudomonas aeruginosa due to the need to reduce the likely contact of the latter with a modern and powerful antibiotic. This prevents the risk of developing drug-resistant bacteria. Tazobaktam exhibits the greatest efficacy against pseudomonas infection. Occasionally, "Piperacillin" or "Clavulanate" is used as the latest generation of antibiotics for pneumonia caused by a hospital strain of the pathogen.
Also on this list are no antibiotics.The latest generation of natural and antistaphylococcal penicillins. The former cannot be used in outpatient treatment because of the need for frequent intravenous or intramuscular administration. Forms that allow you to take them orally, does not exist. A similar situation exists with cephalosporins. Having the same spectrum of activity as penicillins, they cannot be administered orally due to destruction in the stomach.

Cephalosporins and parenteral penicillinsapplications are effective last-generation antibiotics for pneumonia. The scientists of the National Academy of Sciences of Belarus have achieved success in the development of the dosage form of their enteral use. However, the results of research have not yet been applied in practice, and preparations of this series can be used so far only in the work of inpatient healthcare institutions.
Highly effective antibiotics for children
Exploring the latest generation of antibiotics,the list of drugs recommended for children is significantly narrowed. In children, only aminopenicillins (Amoxicillin, Clavulanate), cephalosporins (Ceftriaxone, Cefepime), macrolides (Azithromycin, Midekamycin, Roxithromycin, Clarithromycin) can be used. Fluoroquinolone antibiotics, carbapenems and nitrofurans cannot be used due to inhibition of bone growth, hepatic and renal toxicity.
Systemic nitrofurans do not apply due tolack of scientific evidence confirming the safety of treatment. The only exception is "Furacillin", suitable for local treatment of wounds. Modern and highly effective antibiotics for children of the latest generation are as follows: macrolides, penicillins, cephalosporins (the names of the drugs are presented above). The remaining groups of antimicrobial drugs are not recommended because of the toxic effect and impaired skeletal development.
ABS for pregnant women
According to the classification of the FDA (USA), in the treatmentpregnant women can only use some of the latest generation of antibiotics, the list of which is extremely small. They belong to categories A and B, that is, their danger is not confirmed or there is no teratogenic effect in animal studies.
Substances with unproven effects on the fetus, andalso with the presence of a toxic effect, I can be used only in the case of the predominance of the therapeutic effect over the side effects (category C and D). Drugs of category X are distinguished by proven teratogenic effects on the fetus, therefore, if necessary, their use is necessary to terminate a pregnancy.
During pregnancy, the following appliesthe latest generation of broad-spectrum antibiotics in tablets: protected aminopenicillins (Amoklav, Amoxiclav), cephalosporins (Cefazolin, Ceftriaxone, Cefepime). Macrolides (Azithromycin, Clarithromycin, Midekamitsin, Roxithromycin) are allowed to be used in the third trimester of gestation due to the fact that their teratogenic effect has not yet been fully studied, and its absence cannot be said for sure. Also in pregnant women it is safe to use penicillin antibiotics in the absence of allergy.
The use of antibiotics in the treatment of bronchitis
All the latest generation of antibiotics widespectrum of action, theoretically, can be used for bronchitis and pneumonia, if their pharmacodynamic characteristics are optimal for this. However, there are optimal schemes for the rational treatment of such diseases. They take into account options for successful combinations of antimicrobials with a view to a wide coverage of microbial strains.
Nitrofurans, derivatives of nitroimidazole andsulfonamides irrational use in inflammatory diseases of the respiratory system. The most successful combination for bronchitis or pulmonary pneumonia is protected aminopenicillin with a macrolide (Amoclav + Azithromycin). Prolonged bronchitis requires the appointment of cephalosporin instead of aminopenicillin ("Ceftriaxone" + "Azithromycin"). In this scheme, the macrolide can be replaced by another class analogue: Midekamycin, Clarithromycin, or Roxithromycin.

Все указанные антибиотики последнего поколения with bronchitis have a pronounced effect, although the clinical signs of the disease may continue to be present. The criterion for the effectiveness of treatment is the appearance of cough with phlegm gradually cleared and the relief of fever. With COPD, shortness of breath also decreases, appetite improves, and the frequency of cough urges decreases.
Effective treatment of pneumonia
Mild pneumonia is treated according to the principlebronchitis, but with the use of cephalosporin and macrolide. For moderate to severe pneumonia of non-hospital origin, cephalosporin (Ceftriaxone or Cefepime) is prescribed with a representative of a number of fluoroquinolones (Cyprofloxacin or Levofloxacin). These antibiotics of the latest generation of broad-spectrum suppress the extrahospital microflora well, and the effect of their use is noticeable on the second day of treatment.
Modern antibiotics of the last generationpneumonia (the names are presented above) affect the pathogen, suppressing its vital activity or killing it. The first substances are called bacteriostatic, and the second bactericidal drugs. Cephalosporins, aminopenicillins and fluoroquinolones are bactericidal substances, and macrolides are bacteriostatic. Moreover, the combination of antibiotics aims not only to expand the spectrum of activity, but also to observe the rules of combination: one bactericidal drug with one bacteriostatic.
Treatment of severe pneumonia in ICU
In intensive care where they can bepatients with severe pneumonia and distress syndrome on the background of intoxication. The main contribution to the severity of the condition of such patients is made by pathogenic microflora that is resistant to most antimicrobials. In such situations, use carbapenems ("Imipinem-cilastatin", "Tien", "Meropenem"), unacceptable for use on an outpatient basis.
Treatment of sinusitis and sinusitis
Modern antibiotics of the last generationantritis or sinusitis are used to kill germs. In such cases, a single bactericidal antibiotic can be used. However, in case of antritis, the main difficulty is access of the antimicrobial drug to the site of inflammation. Therefore, the most commonly used drug cephalosporin series. An example is Ceftriaxone or Cefepime. Fluorquinolone III generation - Levofloxacin may also be administered.
Treatment of angina with modern antimicrobial agents
Last generation antibiotics for sore throatappointed with the same purpose. Moreover, the same antimicrobial agents can be used with sinusitis and tonsillitis. The only difference is that in the case of inflammation of the tonsils, antiseptics can also be used, for example, "Furacilin" - a preparation of a number of nitrofurans. Although in case of angina, aminopenicillins protected by sulbactam or clavulanic acid (Amoklav, Amoxiclav, Ospamox) can also be used successfully. Moreover, drugs should be prescribed for 10-14 days.

Treatment of pyelonephritis and urinary tract infections
Due to urinary tract contaminationmicrobes, the latest generation of antibiotics for pyelonephritis are necessary for their treatment. Cephalosporins, fluoroquinolones and nitrofurans have the greatest therapeutic value. Cephalosporins are used for a relatively mild course of pyelonephritis, and fluoroquinolones (Ciprofloxacin, Levofloxacin, Ofloxacin, Moxifloxacin) - for a worsening condition against the background of ongoing therapy.
The most successful drug, suitable for bothmonotherapy, and for combination with Ceftriaxone, is any representative of a number of nitrofurans - “Furamag”). Quinolone - nalidixic acid may also be used. The latter create high concentrations in the urine and act actively against urinary tract pathogens. Also, occasionally, metronidazole is used for vaginal dysbacteriosis and vaginal dysbacteriosis.
Drug resistance and its effect

Due to the constant change of geneticthe material of microorganisms, mainly bacteria, the effectiveness of many antimicrobials is significantly reduced. By acquiring drug resistance, bacteria acquire the ability to survive in the human body, mediating deterioration in infectious diseases. This forces researchers to search for and introduce new antibiotics of the last generation into practice.
Total for the period of existence of antimicrobialabout 7000 substances have already been developed, which are definitely used in medicine. Some of them came out of use because of clinically important side effects or due to the acquisition of resistance by microbes against them. Therefore, about 160 drugs will be applied in medicine today. About 20 of them are the latest generation of antibiotics, the names of which often appear in medical guidelines on antimicrobial treatment of infectious diseases.








