As it was found out in the recent past, besidesobvious functions of the heart also performs the role of the internal secretion organ. This aroused interest not only among medical theorists, but also among practitioners. Natriuretic peptides (NUP) are isolated not only in the myocardium, but also in a number of other internal organs that had not previously discredited endocrine functions. It was a collective decision to use quantitative indicators of LUP in the blood to predict the development of heart disease, since this method was the least invasive and simple for the patient.
Opening the endocrine function of the heart
Natriuretic peptides were discovered back ineighties of the last century, when scientists observed a link between the stretching of the heart chambers and the intensity of urine secretion. The authors of the discovery initially considered this phenomenon to be a reflex and did not give it any significance.
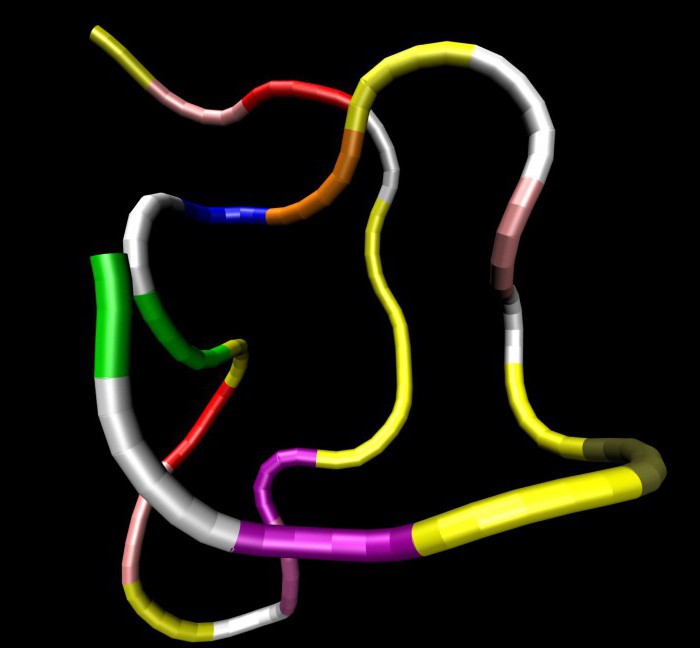
Later, when the study of this issue tookpathologists and histologists, they found out that in the cells of the tissue that makes up the atria, there are inclusions containing protein molecules. It has been experimentally proven that an extract from rat atria produces a powerful diuretic effect. Then it was possible to isolate the peptide and establish the sequence of amino acid residues that make it up.
Еще некоторое время спустя биохимики выделили в This protein has three separate components (alpha, beta and gamma), which differ not only in chemical structure, but also in their effects: alpha was stronger than the other two. Currently distinguished:
- Atrial NUP (type A);
- cerebral LUP (type B);
- urodilatin (type C).
Biochemistry of natriuretic peptide

All natriuretic peptides are similar in theirstructure and differ only in terminal nitrogenous radicals or the arrangement of carbon atoms. To date, all the attention of chemists is concentrated on LLP type B, as it has a more stable form in the blood plasma, and also provides more informative results. Atrial NUP plays the role of one of the correctors of water and electrolyte balance of the body. It is produced in the myocardium both in normal conditions and on the background of chronic heart failure.
It is proved that the precursor of the cerebral NUPconsists of 108 amino acid residues synthesized by the cells of the left ventricle. When the molecule is detached from the cytoplasm, it is affected by the enzyme furin, which turns the protein into an active form (32 amino acids out of 108). Brain NUP exists in the blood just 40 minutes, after which it decomposes. Increased synthesis of this protein is associated with increased stretching of the walls of the ventricles and heart ischemia.
Removal of NUP from plasma is carried out in two main ways:
- cleavage by lysosomal enzymes;
- proteolysis.
The leading role is assigned to the effect on the molecules of neutral endopeptidase, however both methods contribute to the elimination of natriuretic peptides.
Receptor system

All effects of natriuretic peptidescarried out due to their interaction with receptors located in the brain, blood vessels, muscles, bone and adipose tissue. Equivalent to the three types of LLP, there are three types of receptors - A, B and C. But the distribution of "duties" is not so obvious:
- Type A receptors interact with atrial and cerebral NUP;
- B-type responds only to urodilatin;
- C receptors can bind to all three types of molecules.
Receptors are fundamentally different from each other.A- and B-types are designed to realize the intracellular effects of the natriuretic peptide, and type C receptors are necessary for the biodegradation of protein molecules. There is an assumption that the impact of cerebral NUP is carried out not only through type A receptors, but also with other perceiving sites that respond to the amount of cyclic guanosine monophosphate.
The greatest number of type C receptorsfound in brain tissue, adrenal glands, kidneys and blood vessels. When the LUP molecule binds to the type C receptor, it is absorbed by the cell and splits, and the free receptor returns to the membrane.
Physiology of the natriuretic peptide

Brain and atrial natriuretic peptidesrealize their effects through a system of complex physiological reactions. But they all eventually lead to the same goal - reducing the preload on the heart. LUP affects the cardiovascular, endocrine, excretory and central nervous system.
Since these molecules have affinity for differentreceptors, it is difficult to isolate the effects that certain types of LLP have on a particular system. In addition, the effect of the peptide depends not so much on its type, as on the location of the receptor receptor.
Atrial natriuretic peptide refers tovasoactive peptides, that is, directly affects the diameter of the vessels. But besides this, it is able to stimulate the production of nitric oxide, which also contributes to the expansion of blood vessels. LLP A-type and B-type have the same effect and directionality on all types of vessels, and C-type significantly expands only veins.
Recently, the opinion has been expressed thatneed to be perceived not only as a vasodilator, but mainly as an antagonist of vasoconstrictors. In addition, there are studies that prove that natriuretic peptides affect the distribution of fluid inside and outside the capillary network.
Renal effects of natriuretic peptide

About the natriuretic peptide can be said thatIt is a diuresis stimulant. First of all, NUP type A increases the renal blood flow and increases the pressure in the glomerular vessels. This, in turn, increases glomerular filtration. At the same time, CUP type C enhance the excretion of sodium ions, and this leads to even greater water loss.
With all this any significant changesystemic pressure is not observed, even if the level of peptides is increased several times. All scientists agree that the effects that natriuretic peptides have on the kidneys are necessary for correcting the water-electrolyte balance in chronic pathologies of the cardiovascular system.
Effect on the central nervous system
Brain natriuretic peptide, likeatrial, can not penetrate the blood-brain barrier. Therefore, they affect the structures of the nervous system located outside it. But at the same time, some of the LLPs are secreted by the membranes of the brain and other parts of it.
Central effects of natriuretic peptideslie in the fact that they reinforce the already existing peripheral changes. So, for example, along with a decrease in the preload on the heart, the body reduces its need for water and mineral salts, and also the tone of the autonomic nervous system changes in the direction of its parasympathetic part.
Laboratory markers

The idea of taking the natriuretic peptide for analysisThe time of the cardiovascular system malfunction arose in the early 90s of the last century. A decade later, the first publications appeared with the results of research in this area. It was reported that NPU type B is informative in assessing the severity of heart failure and predicting the course of the disease.
Protein content is determined in whole venousblood mixed with ethylenediaminetetraacetic acid, or by immunochemical analysis. Normally, the level of NUP should not exceed 100 ng / ml. In addition, you can determine the level of the predecessor of the LLP using the electrochemiluminescence method. Domestic medicine, not having such a diversity, uses ELISA as a universal means for determining the amount of a substance in the blood serum.
Determination of heart dysfunction

Natriuretic peptide (normal - up to 100 ng / ml)at the moment is the most popular and most modern marker for determining the dysfunction of the heart muscle. The first studies of peptides were associated with difficulties in differentiating chronic circulatory failure and chronic obstructive pulmonary disease. Since the clinical symptoms were similar, the test helped to identify the cause of the ailment and predict the further development of the disease.
The second pathology that has been studied withof this angle, has become ischemic heart disease. The study authors agree that determining the level of LLP helps to establish the estimated level of mortality or relapse in a patient. In addition, dynamic LUP level tracking is a marker of treatment effectiveness.
Currently, the level of NUP is determined in patients with cardiomyopathy, hypertension, stenosis of the great vessels and other circulatory disorders.
Use in cardiac surgery
Empirically, it was found thatAtrial natriuretic peptide in the blood can be considered as an indicator of the severity of the state and work of the left ventricle in patients before and after heart surgery.
The study of this phenomenon began in 1993,but great scope reached only in the 2000s. It was found that a sharp decrease in the number of LUP in peripheral blood, if before that its level was constantly raised, indicates that myocardial function is restored and the operation was successful. If there was no reduction in LLP, then the patient died with a 100% chance. The relationship between age, sex and peptide level was not identified, therefore, this indicator is universal for all categories of patients.
Prediction after surgery
Before heart surgerynatriuretic peptide increased. After all, if it were otherwise, then there was no need for treatment either. A high level of LUP in patients before treatment is an adverse factor that strongly affects the prognosis after surgery.
Since the group selected for the study wasnot numerous, the results were mixed. On the one hand, determining the level of LLP before and after the operation allowed doctors to predict what kind of medical and instrumental support the heart will need until its functions are fully restored. It has also been observed that an increased amount of type B LLP is a precursor of atrial fibrillation in the postoperative period.










