Different blood types have a number of distinctivecomponents that can negatively affect the combination of two different groups. This phenomenon is explained by the presence on the surface and in the plasma of each separate group of an individual combination of agglutinins and agglutinogens, which are able to distinguish a foreign erythrocyte from its own, prevent it functioning inside the body.Human immune system cells with a foreign agglutinogen are perceived as a threat. And for protective purposes, the body seeks to damage and remove them with the help of agglutinins contained in the plasma of their red blood cells.
Even before the beginning of the 20th century, it was believed that combiningyou can any blood that was fundamentally wrong. And sometimes it all ended even lethal, since the blood transfused was not perceived by the body. Developed the bonding and destruction of red blood cells. But thanks to K. Landsteiner, who was able to detect and prove the presence of agglutinogens and agglutinins in erythrocytes, blood types are now distinguished, and the blood transfusion scheme has become safe.

Blood types
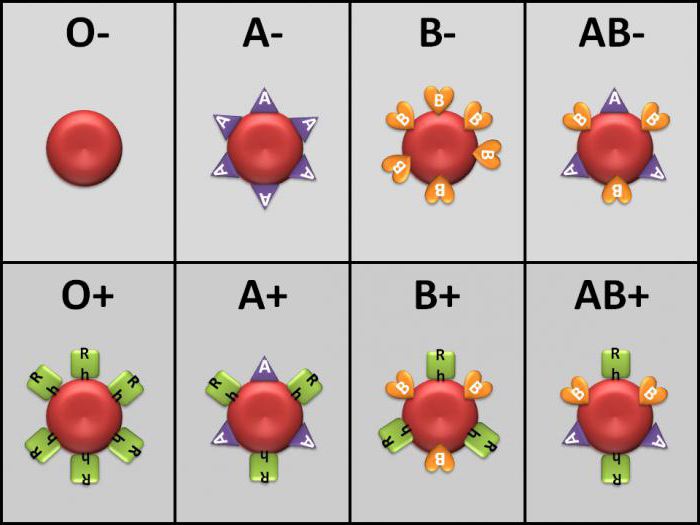
The system developed by Landsteiner is called ABO. Four blood groups are classified according to it, depending on the agglutinogens, denoted A and B, and agglutinins a, b in the composition.
Agglutinogens (antigen) - complex substances located on the erythrocyte membrane, are unchanged and hereditary from parents.
Agglutinin (antibodies) - immunoglobulins,produced in the plasma of erythrocytes in a natural way to protect the body from genes that are absent on the surface of the erythrocyte. They are produced during the first year of life, as a protective function of the immune system against the ingress of proteins with foreign antigens.
| Blood type | Agglutinogen | Agglutinin |
| I group | - | a and b |
| Group II | A | at |
| III group | AT | a |
| Group IV | A and B | - |
As can be seen from the table, each blood group is the difference with a set of antigens and agglutinins that have been developed to the missing antigens for protection.

Blood rhesus factor
In the scheme of blood transfusion acceptable groupscombination also needs to consider the Rh blood. The Rh factor is a constant characteristic that does not change over the course of life and is a classification of blood according to the Rhesus system (Rh). The Rh system is based on the detection of six antigens C, D, E, c, d, e on the surface of red blood cells, was discovered in 1940 by K. Landsteiner and A. Weiner.
If an antigen is found on the surface of the red blood cellsD (occurs in 80% of people) or the simultaneous presence of antigens C and E, then blood belongs to the positive Rh factor, denoted Rh +. If the antigens of this group are not detected, then the Rh factor will be negative Rh-.

Significance of Rh factor during transfusion
For transfusion, blood is allowedsimilar values in the Rhesus system. So, a donor's blood of a negative indicator will be suitable for a recipient with a negative Rh factor. It is the same with positive, however in critical cases blood infusion with negative Rh factor in small quantities is allowed, maximum 200 ml. With such a transfusion, incompatibility does not occur, but when the erythrocyte is positively injected into the blood with a negative Rh factor, a protective response of the immune system to the antigen D is observed. infused red blood cells, which entails serious consequences for the body of the recipient. According to the Rhesus system and ABO, there are eight types of blood.
Blood compatibility
Blood transfusion - blood transfusion procedurewhich is used to restore blood balance and blood circulation. Donated blood must be compatible with both blood systems in the recipient’s blood. For a long time it was believed that there was a universal donor and universal recipient. At the moment, both of these concepts are already practically extracted from the medical system. However, in critical situations, in the absence of time and donor blood of an identical group and Rh factor, it is sometimes used in transfusions of small volumes, not more than 500 ml.
To the universal donor include the blood of the firstgroup and a negative value of rhesus 0 (I) Rh-, since its composition does not have its own antigens. The fourth positive AB (IV) Rh + group is considered a universal recipient, due to the presence of antigens A and B on the erythrocyte membrane. But, nevertheless, they try to carry out the transfusion procedure with identical groups.

Blood type I: compatibility scheme
During transfusion, I group with negativethe value of the rhesus (0 (I) Rh-) can be a donor for all blood groups with a positive and negative Rh factor during emergency transfusion and, if necessary, a large volume to act as a donor for the I group with identical rhesus.
For the recipient with the first blood group andRh-positive donor blood may be the first positive or negative group 0 (I) Rh - / +. In the first blood group with a negative rate of rhesus, transfusion is performed only with an identical group of 0 (I) Rh-.
Compatibility of the second group
The second negative group A (II) Rh- may becomedonor for the second and fourth with any indicator of rhesus. The second positive group A (II) Rh + is used as a donor only for the second and fourth AB (IV) Rh + with a positive Rh factor.
The recipient with the second positive groupA (II) Rh + can take donor blood of the first 0 (I) Rh - / + and the second group A (II) Rh - / + with any rhesus indicator. If the recipient's blood is indicated by a negative Rh value. And (II) Rh- transfusion is performed with groups, as for the second positive, only the negative Rh factor value.
Compatibility of the third group
As a donor third blood group with a positive Rh factor B (III) Rh +
used for transfusions to recipients withthe third and fourth group with a positive rate of rhesus. The third negative group is compatible for donation with the third and fourth blood groups, for any value of the Rh factor in the recipient.
Owners of the third positive grouptransfuse donor blood of the first and third groups with negative or positive rhesus. The third negative is characterized by compatibility with the third and fourth group with a negative Rh factor.
Compatibility of the fourth group
Donor blood of the fourth group with a positiveRh factor is only suitable for transfusion to recipients with an identical group and rhesus index. The fourth negative is compatible for transfusion also only in the fourth group with negative and positive rhesus.
But the recipient with the fourth positive groupAB (IV) Rh + is universal and, with a positive rhesus value, perceives absolutely all blood groups with any rhesus values. With a negative Rh factor, when transfusing, donor erythrocytes of all groups are used only with a negative Rh index.

Risks of transfusion of incompatible groups
The main risk of blood transfusion is agglutination.
Agglutination - the process of gluing red blood cells,which leads to their destruction develops when blood enters the body with an agglutinogen, to which the recipient's blood has developed agglutinin. This means that agglutination occurs when the blood is combined with the same antigens and agglutinins A and a, B and b. With this combination, antibodies (a or b) produced for the missing antigen (A or B) destroy the donor red blood cells, resulting in their sedimentation and subsequent hemolysis (disintegration).

The ABO and Rhesus system is essential whenclassification, but not the only one. On the surface of the erythrocyte membrane, there are many other antigens that are currently involved in the selection of compatible donor blood. But, more and more private clinics additionally determine the presence or absence of a rare Kell antigen, with a positive value of which donor red blood cells are incompatible with any other.









